Total Knee Replacement
Introduction
Total Knee Replacement (TKR) is a common procedure for knee arthritis. We are the only hospital in Malaysia with a Joint Replacement Program (JRP) where you will receive dedicated care throughout your journey with us.
In an Arthritic Knee
- The cartilage lining is thinner than normal or completely absent. The degree of cartilage damage and inflammation varies with the type and stage of arthritis.
- The capsule of the arthritic knee is swollen
- The joint space is narrowed and irregular in outline; this can be seen in an X-ray image.
- Bone spurs or excessive bone can also build up around the edges of the joint The combinations of these factors make the arthritic knee stiff and limit activities due to pain or fatigue.
Diagnosis
The diagnosis of osteoarthritis is made based on history, physical examination & X-rays.
Benefits
The decision to proceed with TKR surgery is a cooperative one between you, your surgeon, family and your local doctor. The benefits following surgery include relief from:
- Severe pain that limits your everyday activities including walking, shopping, visiting friends, getting in and out of chair, gardening, etc.
- Pain waking you at night
- Deformity- either bowleg or knock knees
- Stiffness
Prior to surgery you will usually have tried some conservative treatments such as simple analgesics, weight loss, anti-inflammatory medications, physical therapy or modification of your activities, for example using a cane to walk.
If the above treatments or lifestyle modifications do not offer long-lasting solution, surgery could be your next option. Most patients who have TKR are between 55 to 80 years of age. However each patient is assessed individually and occasionally patients as young as 20 or as old as 90 are also operated on with good results.
Pre-Operation
- Your surgeon will send you for routine blood tests and any other investigations required prior to your surgery
- You will be asked to undertake a general medical check-up with a physician
- You should have any other medical, surgical or dental problems attended to prior to your surgery
- You will attend our special Joint Replacement Program and Classes.
- You will need to make arrangements for help around the house prior to surgery
- You should cease aspirin or anti-inflammatory medications 10 days prior to surgery as they can cause bleeding
- You should cease any naturopathic or herbal medications 10 days before surgery
- You should stop smoking prior to surgery
Day of your surgery
- You will be admitted to the hospital, usually on the same day or the day before surgery
- Further tests may be required on admission
- You will meet the nurses and answer some questions for the hospital records
- You will meet your Anesthetist, who will ask you a few questions
- You will be given hospital clothes to change into and have a shower prior to surgery
- The operation site will be shaved and cleaned
- Approximately 30 minutes prior to surgery you will be transferred to the operating room
Surgical Procedure
Each knee is unique and we take this into account by offering different implant sizes for your knee. You may also be a candidate for robotic knee replacement surgery which offers more precision and better outcomes. You can discuss this with your orthopaedic surgeon.
Surgery is performed under sterile conditions in the operating room under spinal or general anesthesia. You will be on your back and a tourniquet may be applied to your upper thigh to reduce blood loss. Surgery takes approximately two hours.
The surgeon cuts down to the bone to expose the bones of the knee joint. The damaged portions of the femur and tibia are then cut at the appropriate angles using specialized jigs or a specialized robot. Trial components are then inserted to check the accuracy of these cuts and determine the thickness of plastic required to place in between these two components. The patella (knee cap) may be replaced depending on a number of factors.
The real components are then inserted with or without cement and the knee is again checked to make sure things are working properly. The knee is then carefully closed with stitches and the knee dressed and bandaged.
Post-Operative Course
When you regain consciousness, you will be in the recovery room with intravenous drips in your arm, a tube (catheter) in your bladder and a number of other monitors to check your vital signs. You may have a button to press for pain medication through a machine called a PCA machine (Patient Controlled Analgesia).
Once stable, you will be taken to the ward. The post-op protocol is surgeon dependent, but in general you will sit out of bed and start moving you knee and walking within a day or two of surgery. The dressing will be reduced the next morning to make movement easier. Your rehabilitation and mobilization will be supervised by a physical therapist.
To avoid lung congestion, it is important to breathe deeply and use a triflow which will be provided to you. Your orthopaedic surgeon will use one or more measures to minimize blood clots in your legs, such as aspirin, inflatable leg coverings, stockings or injections into your abdomen to thin the blood clots or DVT’s, which will be discussed in detail in the complications section.
The long term results of knee replacements depend on how much work you put into it following your surgery. Usually, you will remain in the hospital for 2-3 days. Then, depending on your needs, either return home or proceed to a rehabilitation facility. You will need physical therapy on your knee following surgery. You will be discharged with a walker and will usually progress to a cane at six weeks.
Your sutures are sometimes dissolvable but if not, are removed at approximately 10 days. The extent of bending your knee varies, but by 4 weeks your knee should be able bend to 100 degrees. The goal is to obtain 115-125 degrees of movement.
Once the wound is healed, you may shower. You can drive at about 6 weeks, once you have regained control of your leg. You should be reasonably comfortable to walk by 6 weeks. More physical activities, such as sports previously discussed, may take 3 months to do comfortably.
When you go home you need to take special precautions around the house to make sure it is safe. You may need rails in your bathroom or to modify your sleeping arrangements, especially if there are lot of stairs in your house.
You will have regular checkups with your surgeon who will assess your progress. You should continue to see your surgeon regularly to check your knee and take X-rays. This is important as sometimes your knee can feel excellent but there can be a problem only recognized with X-ray.
You are always at risk of infections especially with any dental work or other surgical procedures where bacteria can get into the blood stream and find their way to your knee. If you ever have any unexplained pain, swelling or redness or if you feel generally unwell, you should see your doctor as soon as possible.
Risks and Complications
As with any major surgery, there are potential risks involved. The decision to proceed with the surgery is made because the advantages of surgery outweigh the potential disadvantages. It is important that you are informed of these risks before the surgery takes place.
Complications can be medical (general) or local specific to the knee. Medical complications include anesthetic complications. Almost any medical complication can occur so this list is non-exhaustive.
Complications include:
- Allergic reactions to medications
- Blood loss requiring transfusion with low risk of disease transmission
- Heart attacks, strokes, kidney failure, pneumonia, bladder infections
- Infection or nerve damage due to nerve blocks
Serious medical problems can lead to ongoing health concerns or prolonged hospitalization.
Local Complications
Infection
Infection can occur with any operation. In the knee, this can be superficial or deep. Infection rates vary. If it occurs, it can be treated with antibiotics but might require further surgery. Very rarely your new knee may need to be removed to eradicate infection. At ALTY, we focus on successful outcomes and low infection rate.
Blood Clots (Deep Venous Thrombosis)
Blood clots can form in the calf muscles and can travel to the lung (pulmonary embolism). These can occasionally be serious and even life threatening. If you get calf pain or shortness of breath at any stage, you should notify your doctor.
Stiffness in the Knee
Ideally your knee should bend beyond 120 degrees but occasionally, the knee may not bend as well as expected. Sometimes manipulations are required. This means going back to the operating room where the knee is bent for you while you are and under anesthetic.
Wear
The plastic liner eventually wears out over time, usually 15 to 20 years and may need to be changed.
Wound Irritation or Breakdown
The operation will always cut some skin nerves, so you will inevitably have some numbness around the scar. This does not affect the function of your joint. You can also get some aching around the scar. Vitamin E cream and massaging can help reduce this. Occasionally, you can get reactions to the sutures or a wound breakdown that may require antibiotics or rarely, further surgery.
Cosmetic Appearance
The knee may look different than it was because it has been put back into the correct alignment (straightened) to allow proper function.
Leg length inequality
This is due to the fact that a corrected knee is straighter.
Dislocation
An extremely rare condition where the ends of the knee joint lose contact with each other or the plastic insert can lose contact with the tibia (shinbone) or the femur (thigh bone).
Patella problems
The patella (knee cap) can dislocate. This means it moves out of place and it can break or loosen.
Ligament injuries
There are a number of ligaments surrounding the knee. These ligaments can be torn during surgery or break or stretch out any time afterwards. Surgery may be required to correct this problem.
Damage to Nerves and Blood Vessels
Nerves and blood vessels are rarely damaged at the time of surgery. If recognized they are repaired, but a second operation may be required. Nerve damage can cause a loss of feeling or movement below the knee and can be permanent.
Summary
Surgery is not a pleasant prospect for anyone, but for some people with arthritis, it could mean the difference between leading a normal life or putting up with a debilitating condition. Surgery can be regarded as part of your treatment plan—it will help to restore function to your damaged joints as well as relieve pain.
TKR is one of the most successful operations available today. It is an excellent procedure to improve the quality of life, take away pain and improve function. In general, 90 to 95% of knee replacements survive for 20 years, depending on age and activity level.
Surgery is only offered once non-operative treatments have failed. It is an important decision to make and ultimately it is an informed decision between you, your family, your surgeon and medical practitioner.
Find out more about Total Knee Replacement (TKR) with the following links.
Our Specialists
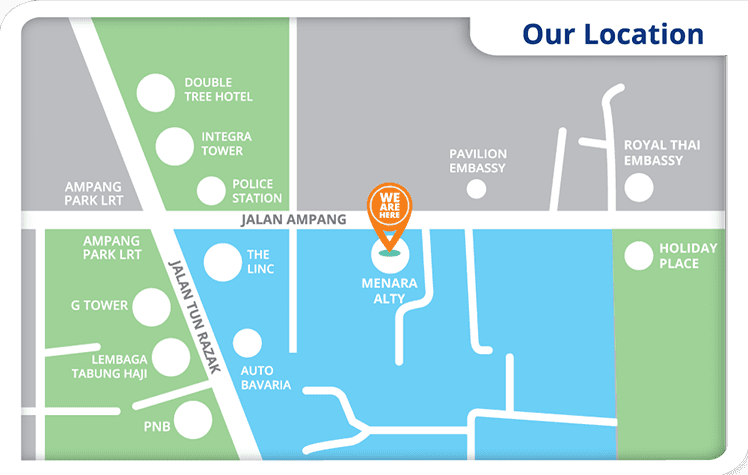
ALTY is the new innovative orthopaedic healthcare provider in Malaysia. Our medical experts work together to provide comprehensive orthopaedic services that best suit your condition and lifestyle. Our team of orthopaedic specialists are trained to utilize advanced technologies to deliver the best patient care and experience.
Meet your surgeons.
Our other specialists in the field of Cardiology, Radiology, and Gastroenterology offer holistic medical care for you, all under one roof.
Meet our medical experts.
 +6012-637 7646
+6012-637 7646 
 DATO' DR. BADRUL SHAH BADARUDDIN
DATO' DR. BADRUL SHAH BADARUDDIN Assoc. Prof. (C) Dr. G Ruslan Nazaruddin Simanjuntak
Assoc. Prof. (C) Dr. G Ruslan Nazaruddin Simanjuntak
 Prof. Dr. Azhar M. Merican
Prof. Dr. Azhar M. Merican DR. SURESHAN SIVANANTHAN
DR. SURESHAN SIVANANTHAN DATO' DR. K.S. SIVANANTHAN
DATO' DR. K.S. SIVANANTHAN Dr. Wong Chung Chek
Dr. Wong Chung Chek DR. LIM SZE WEI
DR. LIM SZE WEI Dr. Lee Chee Kean
Dr. Lee Chee Kean
 Dr. Chew Chin Seong - Visiting
Dr. Chew Chin Seong - Visiting  Dr. Mark Chong
Dr. Mark Chong  DR. PALANI RAMASAMY - Sessional
DR. PALANI RAMASAMY - Sessional  MAJ. GEN. Dato' Dr. Mohammad Amirrudin Hamdan (R) - Visiting
MAJ. GEN. Dato' Dr. Mohammad Amirrudin Hamdan (R) - Visiting Dr. Sanjiv Rampal - Sessional
Dr. Sanjiv Rampal - Sessional
 DR. LYE JUN XIONG - Visiting
DR. LYE JUN XIONG - Visiting  Dr. Juzaily Fekry Leong - Visiting
Dr. Juzaily Fekry Leong - Visiting
 Dr. Syed Muhammad Syafiq Aljunid - Visiting
Dr. Syed Muhammad Syafiq Aljunid - Visiting
 Dr. Faizal Manan Augustin - Visiting
Dr. Faizal Manan Augustin - Visiting
 Dr. Ahmad Fazly bin Abd Rasid - Visiting
Dr. Ahmad Fazly bin Abd Rasid - Visiting
 Dr. Kow Ren Yi - Visiting
Dr. Kow Ren Yi - Visiting
 DR. Leong Yung Chin - Visiting
DR. Leong Yung Chin - Visiting  Dr. Gopinathan Raju - Visiting Consultant
Dr. Gopinathan Raju - Visiting Consultant  Dr. Nik Haziman Wan Hamat
Dr. Nik Haziman Wan Hamat
 Dr. Lee Li Ching
Dr. Lee Li Ching Dr. Mohamad Fadhil Hadi Bin Jamaluddin
Dr. Mohamad Fadhil Hadi Bin Jamaluddin Dr. Sabrilhakim Sidek
Dr. Sabrilhakim Sidek
 Dr. Lim Siu Min
Dr. Lim Siu Min
 DR. ANANTHA KUMAR CHINNASWAMY - Visiting
DR. ANANTHA KUMAR CHINNASWAMY - Visiting  DR. SHAHROL AZMI MOHD YASIN - Visiting
DR. SHAHROL AZMI MOHD YASIN - Visiting  Dr. Dalila bt Yusoff
Dr. Dalila bt Yusoff Dr. Adib Hazizuddin Bin Nasaruddin
Dr. Adib Hazizuddin Bin Nasaruddin Dr. Mohd Lokman Bin Abdul Rahim
Dr. Mohd Lokman Bin Abdul Rahim