Anterior Cruciate Ligament Reconstruction
Introduction
The Anterior Cruciate Ligament (ACL) is one of the major stabilizing ligaments in the knee. It is a strong rope-like structure located in the centre of the knee running from the femur to the tibia. When this ligament tears unfortunately it doesn’t heal and often leads to the feeling of instability in the knee.
ACL reconstruction is a commonly performed surgical procedure. With recent advances in arthroscopic surgery, it can now be performed with minimal incisions and low complication rates.
Function
The ACL is the major stabilizing ligament in the knee. It prevents the tibia (shin bone) moving abnormally on the femur (thigh bone). When this abnormal movement occurs, it is referred to as instability and the patient is aware of this abnormal movement.
Often other structures such as the meniscus, the articular cartilage (lining the joint) or other ligaments can also be damaged at the same time as an ACL injury and these damages to the structures may need to be addressed at the time of surgery.
History of Injury
- Sports related injuries involving a twisting injury to the knee
- Due to a sudden change of direction or a direct blow for example a tackle or landing awkwardly
Often there is a popping sound when the ligament ruptures and the feeling of the knee popping out of the joint. The swelling usually occurs within hours. It is rare to be able to continue playing sports with the initial injury.
Once the initial injury settles down, the main symptom is instability or giving away of the knee. This usually occurs with running activities but can occur on simple walking or other activities of daily living.
Diagnosis
- You can often be diagnosed based on your history alone
- Your examination will reveal the instability of your knee if adequately relaxed or not too painful
- You may undergo an Magnetic Resonance Imaging (MRI) to look for damage to other structures within your knee
- At times, the final diagnosis can only be made under anaesthetic or with an Arthroscopy
Treatment
Initial
- Once you encounter an injury, put your knee at rest
- You may subsequently apply ice to your knee
- Elevate your leg to reduce swelling
- Wrap your knees with bandage to minimise swelling and involuntary movements
Long term
Not everyone needs surgery. Some people can compensate for the injured ligament with strengthening exercises or a brace. If you have an ACL injury, it is strongly advised to give up sports involving twisting activities. Episodes of instability can cause further damage to important structures within the knee that may result in early arthritis.
Indications for surgery
- Young people wishing to maintain an active lifestyle.
- People who play sports involving twisting activities such as soccer, netball, football
- People with dangerous occupations for example policemen, firemen, roofers, construction workers.
It is advisable to have physiotherapy prior to surgery to help you regain motion and strengthen the muscles as much as possible.
Surgery
Surgical techniques have improved significantly over the last decade contributing to reduced complications are quicker recovery than in the past. The surgery is performed arthroscopically. The ruptured ligament is removed and then tunnels (holes) in the bone are drilled to accept the new graft. This graft which replaces your old ACL is taken either from the hamstring tendon or the patella tendon.
The graft is prepared to take the form of a new tendon and passed through the drill holes in the bone. The new tendon is then fixed into your bone with various devices to hold it into place while the ligament heals into the bone (usually 6 months). The rest of the knee can be clearly visualized at the same time and any other damages are dealt with. The wounds then closed often with a drain and a dressing applied.
Post-operation
- Your surgery is performed as a day only procedure or an overnight stay.
- You will have pain medication by tablet or in a drip (Intravenous).
- Any drains will be removed from your knee.
- A splint is sometimes used for your comfort.
- You will be seen by a physiotherapist who will teach you to use crutches and show you some simple exercises to do at home.
- Leave any waterproof dressings on your knee until your post-op review.
- You can put all your weight on your leg.
- Put ice on your knee for 20 minutes at a time, as frequently as possible.
- Post-op review will usually be between 7-10 days after surgery.
- Physiotherapy can begin after a few days or can be arranged at your first post-op visit.
- If you have any redness around the wound, increasing pain in your knee, fever or feeling unwell, you should contact your surgeon as soon as possible.
Rehabilitation
Physiotherapy is an integral part of the treatment and it is recommended to start as early as possible. Preoperative physiotherapy is helpful to better prepare your knee for surgery. The early aim is to help you regain range of motion, reduce swelling and achieve full weight bearing.
The remaining rehabilitation will be supervised by a physiotherapist and will involve activities such as exercise, bike riding, swimming, proprioceptive exercises and muscle strengthening. You can begin cycling at 2 months and jogging can generally begin at around 3 months. The graft is strong enough to allow you do sports at around 6 months however other factors come into play such as confidence, fitness and adequate fitness and training.
Professional sportsmen often return at 6 months but recreational athletes may take 10 -12 months depending on motivation and time put into rehabilitation. The rehabilitation and overall success of your procedure can be affected by associated injuries to the knee such as damage to meniscus, articular cartilage or other ligaments.
The following is a more detailed rehabilitation protocol useful for patients and physiotherapists. It is a guide only and must be adjusted according to your needs taking into account pain, other pathology, work and other social factors.
Acute (0 – 2 Weeks)
Goals
- Wound healing
- Reduce swelling
- Regain full extension
- Full weight bearing
- Wean off crutches
- Promote muscle control
- Keep brace on at all times except when doing your exercises
Treatment Guidelines
- You can reduce pain and swelling with ice, intermittent pressure pump, soft tissue massage and exercise
- Mobilise your patella
- You can perform active range of motion knee exercises, calf and hamstring stretching, contraction (non-weight bearing progressing to standing), muscle control and full weight bearing. You may aim for full extension by 2 weeks. Full flexion will take longer and generally will come with gradual stretching. You need to care for your hamstring co-contraction as this may result in hamstring strains if too vigorous. For the next stage, you can continue with light hamstring loading with progression of general rehabilitation. You should avoid resisted hamstring loading should for approximately 6 weeks
- Gait retraining encouraging extension at heel strike
Stage 2- Quadriceps Control (2-6 Weeks)
Goals
- Full active range of motion
- Normal gait with reasonable weight tolerance
- Minimal pain and effusion
- Develop muscular control for controlled pain free single leg lunge
- Avoid hamstring strain
- Develop early proprioceptive awareness
- Keep brace on at all times except when doing your exercises
Treatment Guidelines
- You can use active, passive and hands-on techniques to promote full range of motion
- You may progress to closed chain exercises (quarter squats and single leg lunge) as pain allows. The emphasis is on pain free loading, VMO and gluteal activation
- Start introducing yourself to gym based exercise equipment including leg press and stationary cycle
- Water based exercises can begin once your wound has healed, including treading water and gentle swimming avoiding breaststroke
- Begin your proprioceptive exercises including single standing leg balance on the ground and mini tramp. This can progress by introducing body movement whilst standing on one leg
- You can do bilateral and single calf raises and stretching
- You should avoid isolated loading of the hamstrings due to ease of tear. Hamstrings will be progressively loaded through closed chain and gym based activity
Stage 3- Hamstring/Quadriceps Strengthening (6-12 Weeks)
Goals
- Begin specific hamstring loading
- Increase total leg strength
- Promote good quadriceps control in lunge and hopping activity in preparation for running
- Remove your brace
Treatment Guidelines
- You may begin focal hamstring loading and progress steadily throughout the next stages of rehabilitation
- Active prone knee flexion which can be quickly progressed to include a light weight and gradually increasing weights
- Bilateral bridging off a chair. This can be progressed by moving onto a single leg bridge and then single leg bridge with weight held across the abdomen
- Single straight leg dead lift initially active with increasing difficulty by adding dumbbells with respect to hamstring loading, they should never be pushed into pain and should be carefully progressed. Any subtle strain or tightness following exercises should be managed with a reduction in hamstring based exercises
- You may perform gym based activity including leg presses, light squats and stationary bike which can be progressively increased in intensity as pain and control allow. It is important to monitor any effusions following exercise and if it is increasing then your exercise should be toned down
- Once single leg lunge control is comparable to the other side, you can introduce hopping. Hops can be made more difficult by including variations such as forward/back, side to side off a step and in a quadrant
- You may begin running towards the latter part of this stage. Prior to running certain criteria must be met:
- No anterior knee pain
- A pain free lunge and hop that is comparable to the other side
- The knee must have no effusion
- Before jogging start having brisk walks, ideally on a treadmill to monitor landing
- Action and any effusion should be done for several weeks before jogging properly
- You may increase proprioceptive manoeuvres with standing leg balance and progressive hopping based activity
- Expand your calf routine to include eccentric loading
Stage Four-Sport Specific (3-6 Months)
Goals
- Improve leg strength
- Develop running endurance speed and change of direction
- Advanced proprioception
- Prepare for return to sports and recreational lifestyle
Treatment Guidelines
- Controlled sports specific activities should be included in your progression of running and gym loads. Increasing effusion post running that isn’t easily managed with ice should result in a reduction in running loads
- You should include advanced proprioception with controlled hopping and turning and balance correction
- You should monitor potential problems associated with increasing loads
- No open chain resisted leg extension exercises unless authorised by your surgeon
Stage Five-Return to Sport (6 Months Plus)
Goals
A safe return to sporting activities
Treatment Guidelines
- Full training for 1 month prior to active return to your competitive sports
- You should prepare for body contact sports. Begin with low intensity one on one contests and progress by increasing intensity and complexity in preparation for drills that one might be expected to do at training
- Improve your running endurance leading up to a normal training session
- Full range, no effusion, good quadriceps control for lunge, hopping and hop and turn type activity. Circumference measures of your thigh and calf to be within 1 cm of other side
Risks & Complications
Complications are not common but can occur. Prior to making the decision of having this operation, it is important you understand these so you can make an informed decision on the advantages and disadvantages of surgery. These can be medical (anaesthetic) or surgical complications
Medical (Anaesthetic) complications
Medical complications include those of the anaesthetic and your general well-being. Almost any medical condition can occur so this list is not complete. Complications include:
- Blood loss requiring transfusion with its low risk of disease transmission
- Heart attacks
- Strokes
- Kidney failure
- Pneumonia
- Bladder infections
- Infection or nerve damage due to nerve blocks
- Ongoing health concerns and prolonged hospitalization.
Surgical complications
The following is a list of surgical complications. These are all rare but can occur. Most are treatable and do not lead to long term problems.
- Infection
Infection can happen in approximately 1 in 200 cases. Treatment involves either oral or antibiotics through the drip, or rarely further surgery to wash the infection out.
- Deep vein thrombosis
These are clots in the veins of the leg. If they occur you may need blood thinning medication in the form of injections or tablets. Very rarely they can travel to your lung (Pulmonary Embolus) which can cause breathing difficulties.
- Excessive swelling & Bruising
This is due to bleeding in your soft tissues and will settle with time.
- Joint stiffness
Can result from scar tissue within your joint, and is minimized by advances in surgical technique and rapid rehabilitation.
- Graft failure
The graft can fail the same as a normal cruciate ligament does. Failure rate is approximately 5%. If your graft stretches or ruptures, it can still be revised if required by using allograft or tendons from your other leg.
- Damage to nerves or vessels
These are small nerves under your skin which cannot be avoided and cutting them leads to areas of numbness in your leg. This normally reduces in size over time and does not cause any functional problems with your knee. Very rarely there can be damage to more important nerves or vessels causing weakness in your leg.
- Hardware problems
All grafts need to be fixed to your bone using various devices (hardware) such as screws or staples. These can cause irritation of your wound and may require removal once the graft has grown into the bone.
- Donor site problems
Donor site means where the graft is taken from. In general, either your hamstrings or patella tendon are used. There can be pain or swelling in these areas which usually resolves over time.
- Residual pain
This can occur especially if there is damage to other structures inside your knee.
- Reflex Sympathetic Dystrophy
An extremely rare condition that is not entirely understood which can cause you unexplained and excessive pain.
Summary
Anterior Cruciate Ligament reconstruction is a common and has a high successful rate. In the hands of experienced surgeons who perform a lot of these procedures, 98% of people have a successful result. It is generally recommended for patients wishing to return to an active lifestyle especially those wishing to play sports involving running and twisting.
The above information hopefully has educated you on the choices available to you, the procedure and the risks involved. If you have any further questions, you should consult your surgeon.
Our Specialists
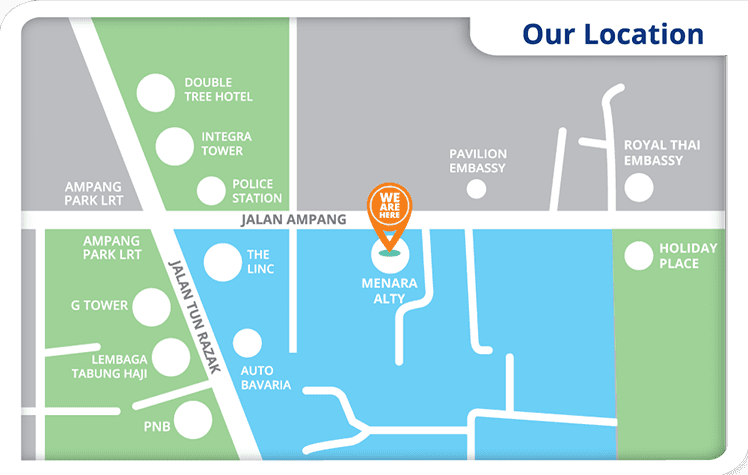
ALTY is the new innovative orthopaedic healthcare provider in Malaysia. Our medical experts work together to provide comprehensive orthopaedic services that best suit your condition and lifestyle. Our team of orthopaedic specialists are trained to utilize advanced technologies to deliver the best patient care and experience.
Meet your surgeons.
Our other specialists in the field of Cardiology, Radiology, Gastroenterology, Urology, ENT and Dermatology offer holistic medical care for you, all under one roof.
Meet our medical experts.
 +6012-637 7646
+6012-637 7646 
 DATO' DR. BADRUL SHAH BADARUDDIN
DATO' DR. BADRUL SHAH BADARUDDIN Assoc. Prof. (C) Dr. Ruslan Nazaruddin Simanjuntak
Assoc. Prof. (C) Dr. Ruslan Nazaruddin Simanjuntak DR. SURESHAN SIVANANTHAN
DR. SURESHAN SIVANANTHAN DR. ANANTHA KUMAR CHINNASWAMY
DR. ANANTHA KUMAR CHINNASWAMY Dr. Ganiga Srinivasaiah Sridhar
Dr. Ganiga Srinivasaiah Sridhar Dr. Lee Li Ching
Dr. Lee Li Ching Dr. Meera Kuppusamy
Dr. Meera Kuppusamy Dr. Mohamad Fadhil Hadi Bin Jamaluddin
Dr. Mohamad Fadhil Hadi Bin Jamaluddin DR. NORZILA TENDOT BT ABU BAKAR
DR. NORZILA TENDOT BT ABU BAKAR DR. PAUL SELVINDOSS
DR. PAUL SELVINDOSS DR. SHAHROL AZMI MOHD YASIN
DR. SHAHROL AZMI MOHD YASIN Dr. Dalila bt Yusoff
Dr. Dalila bt Yusoff DR. LOW LI YAM
DR. LOW LI YAM